Definition of PTSD in Adults – What It Means for Healing
For many adults in California, especially those in Latinx or BIPOC communities, the weight of trauma can feel inescapable long after the actual event is over. Post-traumatic stress disorder alters your sense of safety, affects your relationships, and makes daily life harder. Understanding PTSD as a biological and emotional response to overwhelming experiences is the first step toward finding relief. This overview breaks down what PTSD really is, how its symptoms show up, and how targeted treatments like EMDR therapy can help you move forward.
Table of Contents
Key Takeaways
| Point | Details |
|---|---|
| Understanding PTSD | PTSD arises from traumatic experiences, and its symptoms can vary widely between individuals. Recognizing specific symptom patterns is crucial for effective treatment. |
| Cultural Considerations | Trauma experiences in communities such as Latinx and BIPOC may present unique challenges in recognition and treatment. Culturally informed therapy can enhance recovery outcomes. |
| Treatment Options | Modern treatments, including EMDR and trauma-focused therapies, provide effective pathways for recovery. Personalized treatment plans are essential for addressing individual symptoms and needs. |
| Combatting Stigma | Addressing misconceptions about PTSD is vital. Understanding it as a legitimate health condition helps reduce stigma and encourages individuals to seek help. |
Defining PTSD in Adults: Key Concepts
Post-traumatic stress disorder, or PTSD, is a mental health condition that develops after someone experiences or witnesses a traumatic event. These events can range from natural disasters and serious accidents to violence, assault, or combat exposure. What matters most is not the type of trauma itself, but how your mind and body respond to it in the aftermath. When you encounter genuine danger, your nervous system activates a protective alarm system. This is normal and adaptive. The problem arises when that alarm stays activated long after the threat has passed, creating a state of hypervigilance where your brain continues to perceive danger even in safe situations.
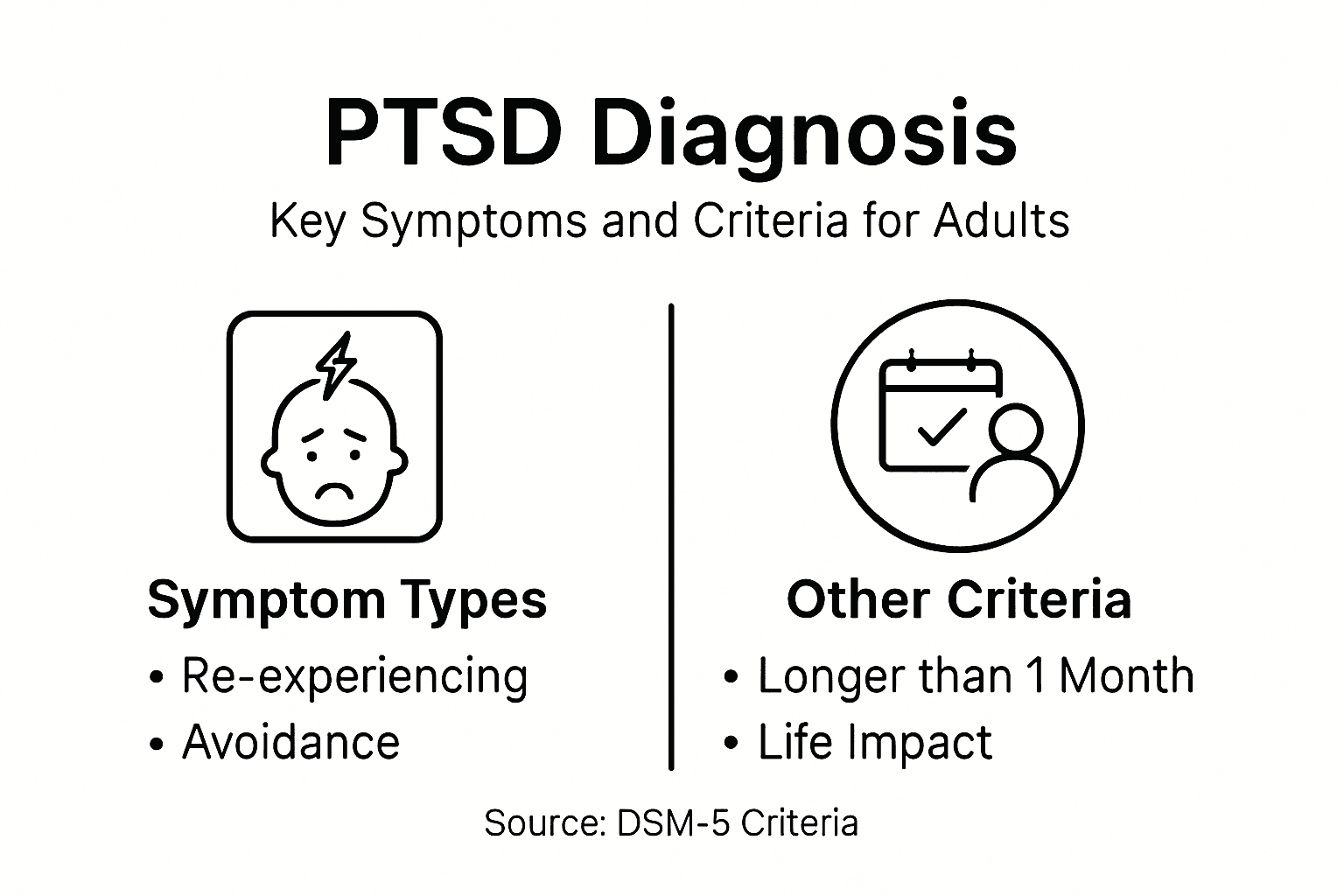
The clinical definition of PTSD involves four specific symptom clusters that mental health professionals use for diagnosis. First, there's re-experiencing, where traumatic memories return unexpectedly through flashbacks, nightmares, or intrusive thoughts that feel as real as the original event. Second, avoidance symptoms develop as your mind tries to escape painful reminders, leading you to avoid certain places, people, or conversations related to the trauma. Third, negative changes in mood and thinking emerge, including difficulty remembering important aspects of the event, persistent negative beliefs about yourself or the world, persistent blame of yourself or others, and emotional numbness. Fourth, changes in arousal and reactivity appear as heightened startle responses, reckless behavior, difficulty concentrating, irritability, and sleep disturbances. These symptoms must persist for more than one month and significantly interfere with your daily functioning at work, home, or in relationships before a diagnosis of PTSD is considered.
What's crucial to understand is that PTSD is not a sign of weakness or failure. Trauma responses occur due to biological changes in how your brain processes fear and stress, combined with social factors and your personal trauma history. Some people develop PTSD after a single traumatic event, while others may experience the same event without developing the disorder. This variation depends on factors including your genetic predisposition, previous trauma exposure, existing mental health conditions, and your support system. Adults in California's Latinx and BIPOC communities often face unique trauma experiences related to immigration, discrimination, or community violence, which can complicate how PTSD manifests and how it's recognized by healthcare providers unfamiliar with culturally specific trauma responses. Healing from PTSD is absolutely possible, and understanding these core concepts is the first step toward recognizing what you're experiencing and seeking appropriate treatment like EMDR therapy or trauma-informed counseling.
Pro tip: Write down your specific symptoms and when they occur most frequently, then bring this record to your first therapy consultation so your clinician can understand your unique trauma presentation and tailor your treatment approach accordingly.
Types and Variations of Adult PTSD
PTSD does not present the same way in every person who experiences trauma. While the core diagnostic criteria remain consistent, the way symptoms show up, their intensity, and which particular symptoms dominate can vary dramatically from one individual to another. Think of PTSD like a fingerprint: the basic pattern is recognizable, but the specific details belong only to you. Someone who witnessed a car accident might be plagued by intrusive flashbacks and startle responses, while another person who survived the same accident might instead struggle primarily with avoidance behaviors and emotional numbness. These differences matter because they affect how treatment gets tailored and what recovery looks like for each person.
One major distinction in how PTSD manifests involves the type and duration of trauma exposure. Direct exposure, where you personally experienced the traumatic event, typically produces different symptom patterns than witnessing trauma or learning about trauma that happened to someone close to you. Additionally, trauma exposure can occur through professional experience, such as what first responders, healthcare workers, and military personnel encounter repeatedly on the job. Another critical variation involves complex PTSD, which develops after prolonged or repeated trauma, particularly during childhood or in situations where escape was impossible. Complex PTSD includes all the standard PTSD symptoms but also adds emotional dysregulation, difficulty maintaining relationships, persistent feelings of detachment, and negative self-perception. Adults in Latinx communities who have experienced immigration trauma, discrimination, or violence may develop complex presentations that blend PTSD with grief and loss.
Research shows that symptom severity and patterns vary significantly based on your genetics, previous trauma history, and current support system. Some adults primarily experience hyperarousal symptoms like anxiety, anger, and sleep disruption. Others lean heavily into avoidance, withdrawing from relationships and activities that once brought them joy. Still others display predominantly negative thinking patterns, believing the world is dangerous or that they are fundamentally damaged. The trajectory of recovery also varies. Some people naturally recover within the first few months after trauma, while others struggle for years without treatment. Your particular constellation of symptoms, their intensity level, and how they interact with your daily responsibilities determine the treatment approach that will work best for your healing journey.
Here is a summary comparing standard PTSD and complex PTSD in adults:
| Feature | Standard PTSD | Complex PTSD |
|---|---|---|
| Trauma Duration | Single or short-term event | Repeated or prolonged trauma |
| Symptom Clusters | Four DSM-5 clusters | DSM-5 clusters plus emotional dysregulation |
| Relationship Difficulties | May occur | More severe and persistent |
| Self-Perception Issues | Less common | Negative, persistent self-beliefs |
Pro tip: When describing your symptoms to a therapist, focus on specific situations that trigger them rather than general statements, since detailed symptom patterns help your clinician identify which PTSD variation you’re experiencing and design the most effective treatment strategy.
Core Symptoms and Diagnostic Criteria
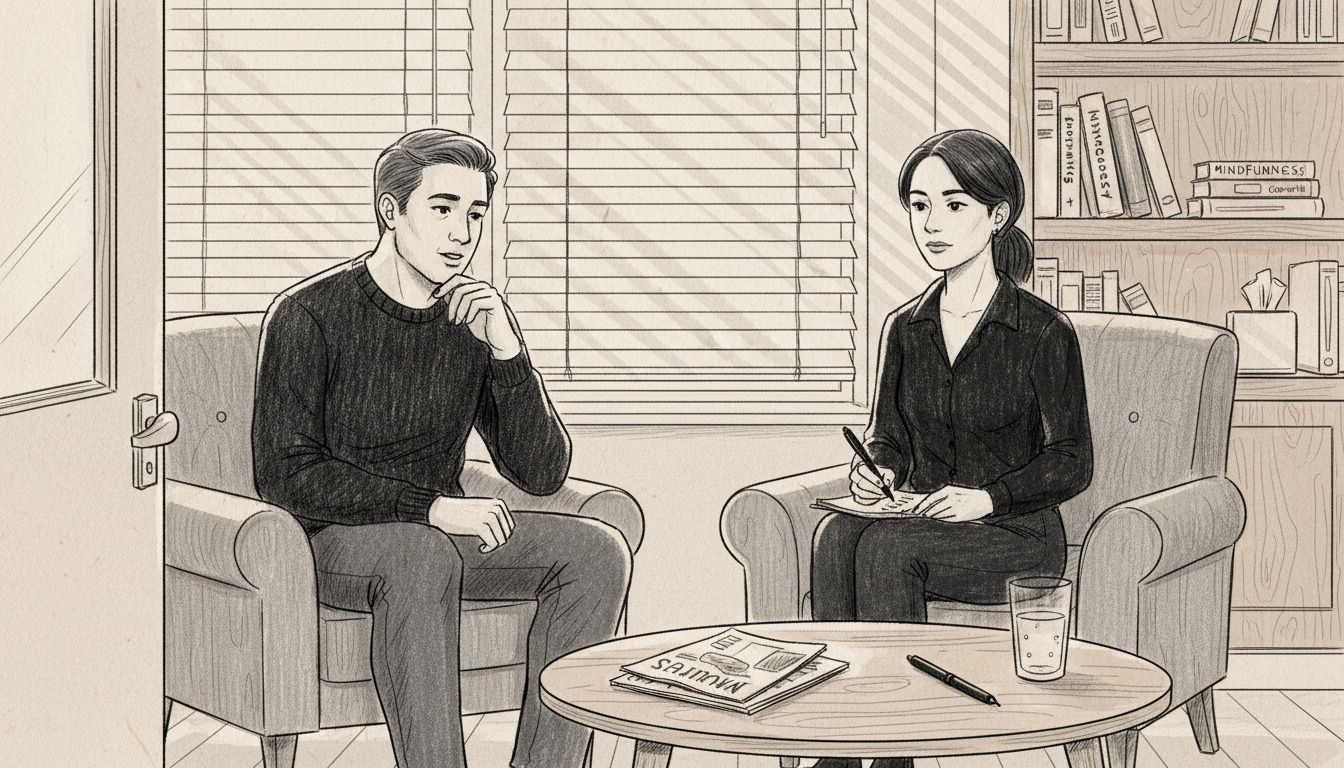
A PTSD diagnosis requires more than just experiencing a traumatic event. Mental health professionals use specific criteria from the DSM-5 to determine whether your symptoms truly constitute PTSD or represent a normal, temporary stress response. Understanding these criteria helps you recognize what you might be experiencing and explains why your therapist asks certain questions during evaluation. The diagnostic process isn't about labeling you but about identifying the exact pattern of your struggles so treatment can address what you actually need.
The core symptoms fall into four distinct clusters. Re-experiencing involves your traumatic memories returning without warning through flashbacks where you feel like the trauma is happening right now, nightmares that jolt you awake in panic, or intrusive thoughts that pop into your mind during everyday activities. Avoidance develops as your mind attempts to escape painful memories by avoiding people, places, conversations, or activities that remind you of the trauma. You might skip social gatherings, change your routes to avoid certain locations, or refuse to talk about what happened. Negative changes in mood and cognition manifest as difficulty remembering key details of the event, persistent negative beliefs about yourself like "I am broken" or "I cannot trust anyone," emotional numbness where you cannot feel pleasure or connection, and persistent blame directed at yourself or others for the trauma occurring. Finally, marked alterations in arousal and reactivity appear as hypervigilance where you constantly scan for danger, an exaggerated startle response to sudden sounds, sleep disturbances, irritability or anger outbursts, and concentration difficulties that make work or schooling challenging.
For a formal PTSD diagnosis, symptoms must persist beyond one month following the trauma and cause clinically significant distress or functional impairment in your work, relationships, or daily activities. You do not need to experience every symptom in every cluster, but you must meet a minimum threshold across the categories. The severity varies considerably. Someone with mild PTSD might manage work but struggle in relationships, while someone with severe PTSD may find leaving their house overwhelming. Additionally, the specific combination of symptoms you experience influences your treatment approach, which is why thorough assessment matters. A skilled trauma-informed therapist will identify your unique symptom profile and customize EMDR therapy or counseling accordingly, rather than applying a one-size-fits-all approach to your healing.
Pro tip: Keep a symptom journal for two weeks before your first therapy appointment, noting when symptoms occur, what triggers them, and how intensely they impact you, since this concrete record gives your clinician precise information that helps establish an accurate diagnosis and baseline for measuring treatment progress.
Misconceptions and Stigma Surrounding PTSD
One of the biggest obstacles to healing from PTSD is not the condition itself, but the shame and misunderstanding that surrounds it. Many people still view PTSD as a sign of weakness, a character flaw, or something that should be "gotten over" with enough willpower. This couldn't be further from the truth. Your brain experiences real, measurable changes after trauma. The neural pathways that process fear and threat detection become overactive. Your stress response system gets stuck in overdrive. These are biological realities, not personal failings. Yet stigma persists, keeping people isolated and preventing them from seeking the help that could transform their lives. The misconceptions run deep, especially in communities where discussing mental health is still considered taboo or where stoicism is culturally valued as a strength.
Common myths about PTSD spread harm in subtle ways. Some people believe PTSD only affects military veterans, when in reality it develops in survivors of domestic violence, sexual assault, car accidents, medical trauma, and countless other experiences. Others assume that talking about trauma makes it worse, when evidence shows that professional counseling approaches help process trauma effectively and reduce symptoms significantly. Some believe you should just "move on" quickly after a traumatic event, not realizing that PTSD develops in the brain's threat detection system and cannot be mentally overridden through willpower alone. Perhaps most damaging is the belief that seeking help is weakness. In reality, reaching out to a trauma-informed therapist demonstrates tremendous courage and self-awareness. Additionally, stigma manifests through negative attitudes and discrimination that create barriers to care, with some people fearing job loss, social rejection, or family judgment if they disclose their PTSD diagnosis.
The good news is that understanding PTSD as a medical condition, not a character issue, is gradually replacing old stigmas. Brain imaging research shows physical evidence of how trauma alters neural function, helping people recognize PTSD as a legitimate health condition deserving compassionate treatment. For Latinx and BIPOC communities in California, cultural healing practices combined with evidence-based therapies like EMDR offer paths to recovery that honor your background while addressing the neurobiological impact of trauma. When you stop internalizing shame about your PTSD and start recognizing it as a treatable condition your nervous system developed to protect you, healing becomes possible. You do not have to suffer in silence or accept the burden of others' ignorance.
Pro tip: When considering therapy, seek out clinicians who explicitly identify as trauma-informed and have experience working with your specific community or trauma type, since cultural competence and specialized training significantly reduce shame and increase treatment effectiveness.
Risks, Impact, and Treatment Pathways
Untreated PTSD does not simply fade away with time. Without intervention, the condition often deepens its roots in your nervous system, creating ripple effects throughout every area of your life. The risks extend beyond emotional suffering. People with PTSD face significantly higher rates of depression, anxiety disorders, and substance use as they attempt to self-medicate the unbearable feelings that accompany their symptoms. Sleep becomes fragmented. Relationships strain under the weight of emotional withdrawal and hypervigilance. Work performance deteriorates. Physical health declines due to chronic stress activation. The longer PTSD remains untreated, the more entrenched these patterns become, and the harder recovery becomes. This is not doom or inevitability, but rather a clear statement of why seeking help early matters profoundly for your future.
The Real-World Impact extends to your entire support network. Your family witnesses your suffering and may feel helpless or confused by behaviors they cannot understand. Children of parents with untreated PTSD can develop their own trauma responses through observing parental anxiety or emotional unavailability. Relationships deteriorate when intimacy becomes impossible due to emotional numbness or hypervigilance. Work relationships suffer when concentration fails and irritability erupts unexpectedly. Communities experience collective trauma when multiple members carry unhealed PTSD from shared experiences like violence, immigration trauma, or discrimination. Yet evidence-based psychotherapies like cognitive processing therapy address trauma at its neurological roots, offering genuine pathways to healing rather than mere symptom management.
Modern treatment options have expanded significantly beyond old approaches that simply asked people to "talk it out." Trauma-focused cognitive behavioral therapy, prolonged exposure therapy, and EMDR (Eye Movement Desensitization and Reprocessing) work by helping your brain reprocess traumatic memories in ways that reduce their emotional charge and restore your sense of safety. For Spanish-speaking and Latinx adults in California, bilingual and culturally responsive trauma therapy honors your specific experiences while addressing the neurobiology of PTSD. Some individuals benefit from medication such as antidepressants working alongside therapy. Early diagnosis and personalized treatment plans significantly enhance recovery outcomes by addressing your unique symptom profile and any co-occurring conditions. The key is finding the right combination of approaches for you, with a therapist who understands both trauma and your cultural context.
Below is a quick reference outlining the main types of modern PTSD treatments and their core benefits:
| Treatment Type | Core Benefit | Notes |
|---|---|---|
| EMDR Therapy | Reprocesses trauma memories | Effective for varied trauma types |
| Cognitive Behavioral Therapy | Reduces negative thoughts and behaviors | Widely used, strong evidence base |
| Prolonged Exposure Therapy | Reduces avoidance and anxiety | Useful for persistent avoidance |
| Medication (e.g., SSRIs) | Alleviates mood and anxiety symptoms | Often combined with psychotherapy |
Pro tip: When exploring treatment options, ask potential therapists about their specific training in trauma therapies like EMDR or cognitive processing therapy, their experience with your type of trauma, and their cultural competence, since specialized expertise directly correlates with faster and more meaningful recovery.
Take Control of Your PTSD Healing Journey Today
Understanding PTSD and its complex symptoms is the first step toward lasting recovery. If you find yourself struggling with intrusive memories, avoidance, or hyperarousal that deeply impact your daily life, you are not alone. At Alvarado Therapy, we specialize in trauma-informed care designed specifically to address PTSD, complex trauma, and the unique challenges faced by adults in California's diverse communities.
Don’t let PTSD define your future. Our licensed therapists offer personalized EMDR therapy, individual counseling, and culturally sensitive support that honors your experiences and identity. Begin your healing journey with a team that understands the biological and emotional nature of trauma and is committed to guiding you toward safety and empowerment. Start now by visiting Alvarado Therapy and explore how our trauma-informed mental health services can help you reclaim your life.
Frequently Asked Questions
What are the key symptoms of PTSD in adults?
The key symptoms of PTSD in adults include re-experiencing traumatic memories, avoidance of reminders of the trauma, negative changes in mood and thinking, and heightened arousal and reactivity. These symptoms must persist for more than one month and significantly impair daily functioning.
How does PTSD differ from complex PTSD?
Standard PTSD typically arises from a single traumatic event, while complex PTSD develops from prolonged or repeated trauma, often during childhood. Complex PTSD includes the same symptoms as standard PTSD but also features emotional dysregulation and persistent relationship difficulties.
Is PTSD a sign of weakness?
No, PTSD is not a sign of weakness. It is a mental health condition that results from biological changes in the brain due to trauma. Seeking help for PTSD demonstrates strength and self-awareness.
What are effective treatments for PTSD?
Effective treatments for PTSD include trauma-focused cognitive behavioral therapy, EMDR (Eye Movement Desensitization and Reprocessing), and prolonged exposure therapy. Some individuals may also benefit from medications such as antidepressants, often in conjunction with therapy.
Recommended
PTSD in Adults – Impact, Symptoms, and Recovery — Alvarado Therapy
How to Manage PTSD Symptoms Naturally and Effectively — Alvarado Therapy
Role of Counseling in PTSD Recovery: Lasting Benefits — Alvarado Therapy
Role of Mindfulness in Therapy: Real Impact on Anxiety and Depression - ReviveHealthTherapy
How Stigma Impacts Substance Abuse Recovery - 12PanelNow | 12 Panel Drug Test | Free Shipping