Difference Between PTSD and C-PTSD – Why It Matters
Sorting through the differences between PTSD and C-PTSD can feel confusing, especially when your trauma began in childhood and still affects your daily life. This matters because a misdiagnosis means you might not get the support your unique story deserves. Discover how each diagnosis relates to your symptoms, relationships, and therapy options, and why understanding your own trauma history is key to building a tailored, effective path toward healing. Disturbances in self-organization set C-PTSD apart, shaping not just your memories but your emotions, self-worth, and connections with others.
Table of Contents
Key Takeaways
| Point | Details |
|---|---|
| Distinction Between PTSD and C-PTSD | Understand that PTSD arises from single traumatic events, while C-PTSD results from prolonged, repetitive trauma, affecting treatment approaches. |
| Symptom Overlap and Differences | Both PTSD and C-PTSD share re-experiencing, avoidance, and hyperarousal symptoms, but C-PTSD includes additional emotional dysregulation and negative self-concept issues. |
| Impact on Relationships | PTSD typically leads to avoidance and hypervigilance, whereas C-PTSD significantly disrupts trust and self-worth across relationships. |
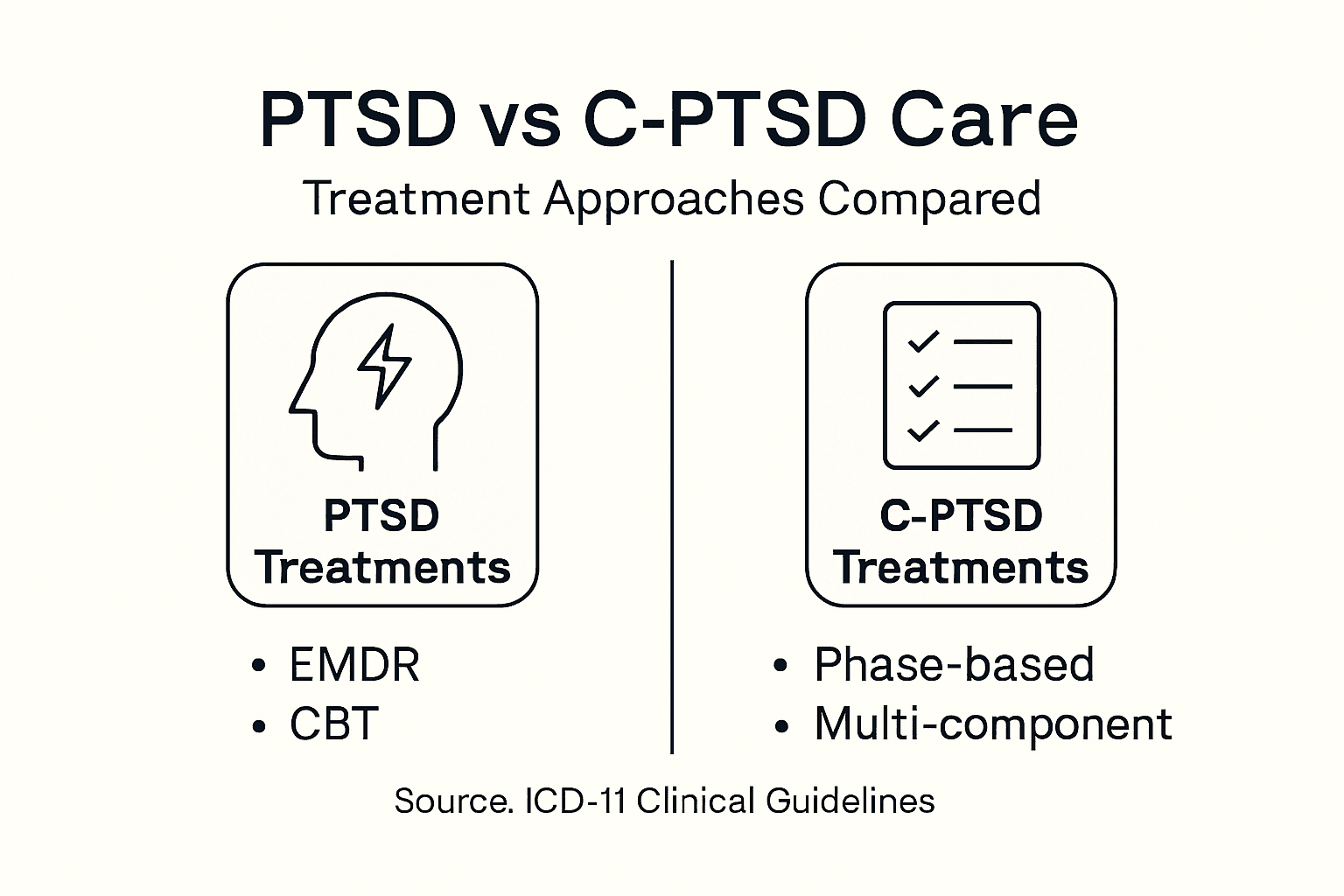
| Tailored Treatment Approaches | PTSD often benefits from direct trauma processing, while C-PTSD requires phased, comprehensive strategies focused on emotional regulation before addressing trauma memories. |
Defining PTSD and C-PTSD Diagnoses
You'll want to understand the key differences between PTSD and C-PTSD because misdiagnosis can significantly impact your treatment path. These are distinct conditions with overlapping symptoms but fundamentally different underlying causes and recovery needs.
PTSD develops after exposure to a single traumatic event or a brief period of intense danger. Think of a car accident, a violent assault, a house fire, or witnessing an injury. Your brain experiences something shocking and overwhelming, and afterward, it struggles to process and store that memory normally. The result is intrusive thoughts, avoidance behaviors, and heightened startle responses that persist long after the event itself has ended.
C-PTSD, by contrast, emerges from prolonged, repetitive trauma that typically occurs during formative years. For many California adults seeking therapy, this means childhood abuse, neglect, or witnessing domestic violence repeatedly. It could also stem from human trafficking, ongoing exploitation, or chronic interpersonal violence in adulthood. The prolonged nature of the trauma fundamentally changes how your brain and nervous system develop, affecting not just how you process memories but how you regulate emotions, view yourself, and connect with others.
Here's what matters clinically: PTSD includes the classic symptom clusters of intrusive memories, avoidance, and hyperarousal. C-PTSD includes all of these plus disturbances in self-organization that look like difficulty managing intense emotions, persistent guilt and shame about who you are, negative beliefs about yourself, and struggles in relationships. You might find yourself unable to trust people, prone to explosive anger over small triggers, or feeling fundamentally broken in ways that extend beyond "I have trauma memories."
The diagnostic recognition matters too. The ICD-11 (used internationally and by many clinicians outside the United States) officially recognizes C-PTSD as a separate diagnosis. The DSM-5, which guides American mental health professionals, does not yet have a standalone C-PTSD diagnosis, though this is changing as research accumulates. This distinction can affect how your therapist understands your condition and which treatment approaches they recommend.
When you're looking at treatment options like EMDR therapy or trauma-focused counseling, knowing whether you have PTSD or C-PTSD helps your clinician tailor the work. Both conditions improve with evidence-based therapy, but the pace, focus areas, and specific interventions may differ based on whether your trauma was single-incident or relational and ongoing.
Pro tip: When meeting with a therapist, explicitly mention if your trauma involved childhood experiences or prolonged interpersonal harm, as this helps them assess whether C-PTSD diagnostics are relevant to your situation.
Distinct Causes and Trauma Histories
The root cause of your trauma fundamentally shapes whether you develop PTSD or C-PTSD. This distinction matters because it explains why your symptoms look different from someone else's and why certain treatments work better for your specific situation.
Single-incident trauma is the hallmark of PTSD. This could be a car accident where you nearly died, a violent assault, a natural disaster, a serious medical emergency, or witnessing someone else get hurt. The key feature is that the traumatic event has a clear beginning and end. Your nervous system experiences acute danger, activates its fight-flight-freeze response, and then the immediate threat passes. What remains is your brain's struggle to process and file away that memory normally. The trauma is discrete. It happened. It's over. Your job in recovery is teaching your brain that you're safe now.
C-PTSD emerges from a completely different trauma landscape. Repeated or sustained traumatic events often begin in childhood and can continue into adulthood. This includes prolonged childhood abuse (physical, emotional, or sexual), chronic neglect, witnessing domestic violence repeatedly, human trafficking, ongoing workplace harassment, or long-term intimate partner violence. The trauma isn't a single shocking event. It's a pattern. Your nervous system never gets to fully relax because the threat keeps returning. You learn that the world isn't safe, that people can't be trusted, and that you have to be hypervigilant to survive.
This extended exposure during formative years changes you differently than acute trauma does. Early-life trauma and C-PTSD share a strong association, particularly when trauma happens during critical developmental periods. Your brain is literally still building its emotional regulation systems, your sense of self, and your capacity to trust others. When trauma happens repeatedly during these windows, it shapes how those systems develop. You might find yourself struggling with emotional intensity that others don't experience, difficulty knowing who you are, or patterns of unhealthy relationships that repeat similar dynamics from your past. How you experienced trauma in childhood often directly influences how you show up in adult relationships.
For California adults who experienced childhood trauma and are now seeking therapy, understanding this difference is crucial. It explains why healing from childhood trauma sometimes requires a different therapeutic approach than treating acute PTSD. Your therapist needs to know whether you're dealing with a single traumatic memory or with deep patterns rooted in how your brain and nervous system organized themselves around years of threat.
Clinically, PTSD can develop from a wider range of single traumatic events, while C-PTSD specifically correlates with prolonged, repetitive harm. Both are real, both cause significant suffering, and both respond to evidence-based treatment. The difference is that your treatment timeline, the focus of your work, and what healing looks like may differ based on these distinct trauma histories.
Pro tip: When sharing your trauma history with a therapist, be specific about the duration and repetition of your trauma, not just the events themselves, as this helps them determine the most appropriate diagnostic framework and treatment strategy for your recovery.
Core Symptoms and Overlapping Features
Both PTSD and C-PTSD share a common foundation of trauma symptoms, which is why they can look similar at first glance. But once you dig deeper, the differences become clear. Understanding what overlaps and what's distinct helps you recognize your own experience and communicate it to a therapist.
The overlapping core symptoms appear in both conditions. Re-experiencing means your traumatic memory keeps showing up uninvited. You might have flashbacks where you feel like you're back in the traumatic moment, vivid nightmares that jolt you awake, or intrusive thoughts that pop into your head when you're just trying to get through your day. A sound, a smell, a location, or even a conversation topic can trigger these memories to surface. Avoidance is your brain's attempt to protect you by steering clear of anything connected to the trauma. You might avoid certain places, people, conversations, or activities. You might numb yourself with substances or compulsive behaviors. Hyperarousal means your nervous system stays on high alert. You're easily startled, sleep poorly, feel constantly on edge, or find yourself angry or irritable over things that wouldn't normally bother you.
These three symptom clusters are necessary for a PTSD diagnosis. If you have PTSD, you definitely experience re-experiencing, avoidance, and hyperarousal. But here's where C-PTSD diverges: it includes all of these plus additional disturbances in self-organization that fundamentally affect how you function. This is the crucial difference.
Affect dysregulation means your emotions are unpredictable and intense. You might swing rapidly from numb to tearful, or from calm to rage. Small frustrations explode into disproportionate anger. You struggle to soothe yourself once you're emotionally activated. Your negative self-concept goes beyond normal self-doubt. You might feel fundamentally broken, unworthy, or bad at your core. You blame yourself for the trauma, carry persistent shame, and struggle to see anything positive about who you are. Relational difficulties show up as trouble trusting people, difficulty maintaining healthy boundaries, or patterns of relationships that echo your trauma history. You might find yourself in cycles where you're either withdrawn and isolated or entangled with people who mistreat you.
Think of it this way: PTSD is like your brain got stuck processing one terrifying file. C-PTSD is like your entire operating system reorganized itself around survival mode. Meeting C-PTSD criteria requires PTSD symptoms plus significant disturbances in self-regulation and identity, creating a broader symptom profile that touches nearly every aspect of how you experience yourself and relate to the world.
What makes this distinction practical for you is that symptom management looks different. Someone with PTSD might benefit greatly from trauma-focused therapy that processes the specific traumatic memory. Someone with C-PTSD often needs to start with stabilization and emotional regulation skills before diving into memory processing, because the emotional dysregulation itself is so destabilizing.
Here's a concise comparison of PTSD and C-PTSD symptom clusters and their impact:
| Symptom Cluster | PTSD Presentation | C-PTSD Presentation | Practical Impact |
|---|---|---|---|
| Intrusive Memories | Flashbacks, nightmares | Flashbacks, nightmares | Difficulty focusing daily |
| Emotional Regulation | Typically intact | Severe affect dysregulation | Challenges managing anger |
| Self-Concept | Temporary negative beliefs | Persistent shame, low self-worth | Isolation, self-blame |
| Relationship Patterns | Specific avoidance patterns | Chronic trust and boundary issues | Difficulty maintaining bonds |
Pro tip: When describing your symptoms to a therapist, mention not just what happened to you but how you function day to day—especially how you regulate emotions, what you believe about yourself, and how you navigate relationships—as these details help identify whether C-PTSD features are present.
Impact on Relationships and Daily Life
Trauma doesn't stay confined to your memories. It ripples outward into how you show up at work, how you connect with partners, how you parent your children, and how you navigate everyday situations. The impact on your relationships and daily functioning differs significantly between PTSD and C-PTSD, and understanding this matters for your recovery.
With PTSD, the relationship impact typically centers around specific avoidance and hypervigilance patterns. You might avoid places or people connected to your trauma. You could struggle with emotional intimacy because talking about feelings feels risky. Hypervigilance means you're constantly scanning for danger, which exhausts you and can make partners feel like they're walking on eggshells. Your partner might not understand why you flinch at loud noises or why you need to sit with your back to the wall at restaurants. But fundamentally, if the trauma wasn't relational in nature, your capacity to connect, trust, and be vulnerable hasn't been shattered at a core level. With treatment, many people with PTSD rebuild their relationships and return to their normal functioning.
C-PTSD creates a different relational landscape. The difficulties in relationships due to affect dysregulation and negative self-beliefs mean trust itself becomes the obstacle. You learned from repeated harm by people who were supposed to protect you that the world isn't safe and that people will hurt you. This doesn't just affect one relationship. It affects how you approach every person. You might sabotage relationships when they get close because you expect betrayal. You might tolerate mistreatment because you don't believe you deserve better. You might oscillate between desperate connection and complete withdrawal. Your partner or family members might feel confused about your emotional intensity, your sudden shifts in mood, or your difficulty believing them when they express care. The shame you carry about who you are can make you isolate even when you desperately need connection.
Beyond relationships, daily functioning takes a hit differently with each condition. PTSD can impair social and occupational functioning through hypervigilance and avoidance, but C-PTSD typically involves more pervasive difficulties across work, school, and personal domains. Someone with PTSD might avoid their workplace parking lot but still perform well once at their desk. Someone with C-PTSD might struggle to show up at all due to emotional dysregulation, difficulty concentrating from persistent shame, or dissociation that makes them feel detached from everything happening around them. They might cycle through jobs because they can't sustain the interpersonal dynamics required. They might have trouble maintaining basic self-care because their negative self-concept tells them they don't deserve to be taken care of.
For California adults working through these issues, this distinction matters when you're trying to understand why therapy or medication alone isn't fixing everything. Your relationships might improve before your internal sense of worth catches up. You might need to actively practice trusting people even when it feels counterintuitive. Recovery is possible for both conditions, but C-PTSD often requires more extensive work in rebuilding your relationship with yourself before you can fully rebuild relationships with others.
Pro tip: Communicate with your therapist about specific relationship struggles and daily functioning challenges, not just trauma symptoms, so they can address both the memory processing and the relational patterns that developed as a result of your trauma history.
Treatment Options and Recovery Pathways
The fact that PTSD and C-PTSD have different causes and symptom profiles means they also respond differently to treatment. Knowing which diagnosis fits your situation helps you and your therapist create a recovery plan that actually addresses what you're dealing with, rather than wasting months on an approach that misses the mark.
PTSD treatment typically focuses directly on the traumatic memory itself. Trauma-focused cognitive-behavioral therapy helps you process what happened by gradually exposing yourself to trauma-related thoughts, feelings, and situations in a safe, controlled way. Your brain learns that the memory itself isn't dangerous, even though it feels that way. Eye movement desensitization and reprocessing (EMDR) uses bilateral stimulation (usually eye movements) while you recall the trauma, which appears to help your brain reprocess and integrate the memory more effectively. Both approaches have strong research support for PTSD. Many people with single-incident trauma see significant improvement within a few months of focused treatment because the goal is clear: process that specific memory and restore your sense of safety.
C-PTSD treatment requires a more complex approach. Multi-component, phase-based treatments addressing both PTSD symptoms and disturbances in self-organization work better than trauma-focused therapy alone. Phase one focuses on stabilization and building emotional regulation skills. You're not diving into trauma memories yet. Instead, you're learning how to manage intense emotions, develop grounding techniques, and create safety in your nervous system. This might include somatic therapy, mindfulness practices, or skills training. Phase two addresses the trauma itself using trauma-focused interventions. But phase three is crucial for C-PTSD: reconnection and identity work. You're literally rebuilding your sense of self, repairing your capacity to trust, and learning healthy relationship patterns. This takes longer than PTSD treatment because you're not just processing memories. You're reorganizing how your brain functions at a fundamental level.
The practical difference shows up in treatment planning. Someone with PTSD might start trauma-focused EMDR or cognitive-behavioral therapy within the first few sessions. Someone with C-PTSD typically needs weeks or months of stabilization work first. Jump into trauma processing before they're ready, and they'll likely become destabilized. Understanding this prevents the frustration of starting therapy, feeling worse, and wondering if treatment is working.
This summary highlights differences in treatment planning for PTSD versus C-PTSD:
| Treatment Focus | PTSD Care Approach | C-PTSD Care Approach | Recovery Timeline |
|---|---|---|---|
| Initial Phase | Trauma memory processing | Emotional stabilization | Weeks for PTSD, months for C-PTSD |
| Therapy Modalities | EMDR, CBT | Multi-phase, skills + trauma | Multiple therapy components |
| Relational Healing | Restore specific bonds | Rebuild trust and identity | Gradual, ongoing work |
Personalized treatment plans combining trauma-focused interventions with strategies targeting emotional regulation and interpersonal difficulties produce the best outcomes for both conditions. This might mean EMDR or trauma-focused CBT for the core trauma, plus skills training for emotion management, plus relational work to rebuild trust and healthy connection patterns. For California adults seeking bilingual, culturally sensitive care, finding a therapist who understands these distinctions and can tailor their approach accordingly makes all the difference in your recovery trajectory.
Pro tip: Ask your therapist explicitly about their phase-based approach and whether they'll assess your emotional regulation capacity before starting trauma-focused work, as this helps ensure your treatment plan matches your specific recovery needs rather than a one-size-fits-all protocol.
Find the Right Support for PTSD and C-PTSD Recovery
Understanding the difference between PTSD and C-PTSD is a crucial step in your healing journey. If you are facing challenges like emotional dysregulation, persistent shame, or difficulty trusting others due to prolonged trauma, you need a therapy approach tailored to your unique experience. At Alvarado Therapy, we specialize in trauma-informed care including EMDR therapy and individual counseling that addresses both single-incident and complex trauma. Our bilingual team is dedicated to creating a culturally sensitive, safe space that honors your story and helps rebuild your sense of self and relationships.
Don't wait to get the personalized care that can change how you live and connect with others. Visit Alvarado Therapy today to learn more about our services including trauma stabilization and trauma-focused treatments. Taking action now means starting your path toward safety, clarity, and empowerment supported by licensed California therapists who understand the complexities of PTSD and C-PTSD.
Frequently Asked Questions
What is the main difference between PTSD and C-PTSD?
PTSD, or Post-Traumatic Stress Disorder, typically develops after exposure to a single traumatic event, while C-PTSD, or Complex Post-Traumatic Stress Disorder, arises from prolonged, repetitive trauma, often occurring during formative years.
What are the key symptoms of C-PTSD that differentiate it from PTSD?
C-PTSD includes all the classic symptoms of PTSD, such as intrusive memories and hyperarousal, but also features disturbances in self-organization, including affect dysregulation, negative self-concept, and relational difficulties.
How does the treatment approach differ for PTSD and C-PTSD?
PTSD treatment usually focuses on processing the specific traumatic memory, often through trauma-focused therapies like EMDR. In contrast, C-PTSD treatment requires a phase-based approach that initially emphasizes emotional stabilization and regulation skills before addressing trauma processing.
Why is it important to accurately diagnose PTSD versus C-PTSD?
Accurate diagnosis is crucial because it affects the treatment plan. Misdiagnosis can lead to inappropriate therapy that may not effectively address the unique needs of each condition, potentially hindering recovery.